Introduction
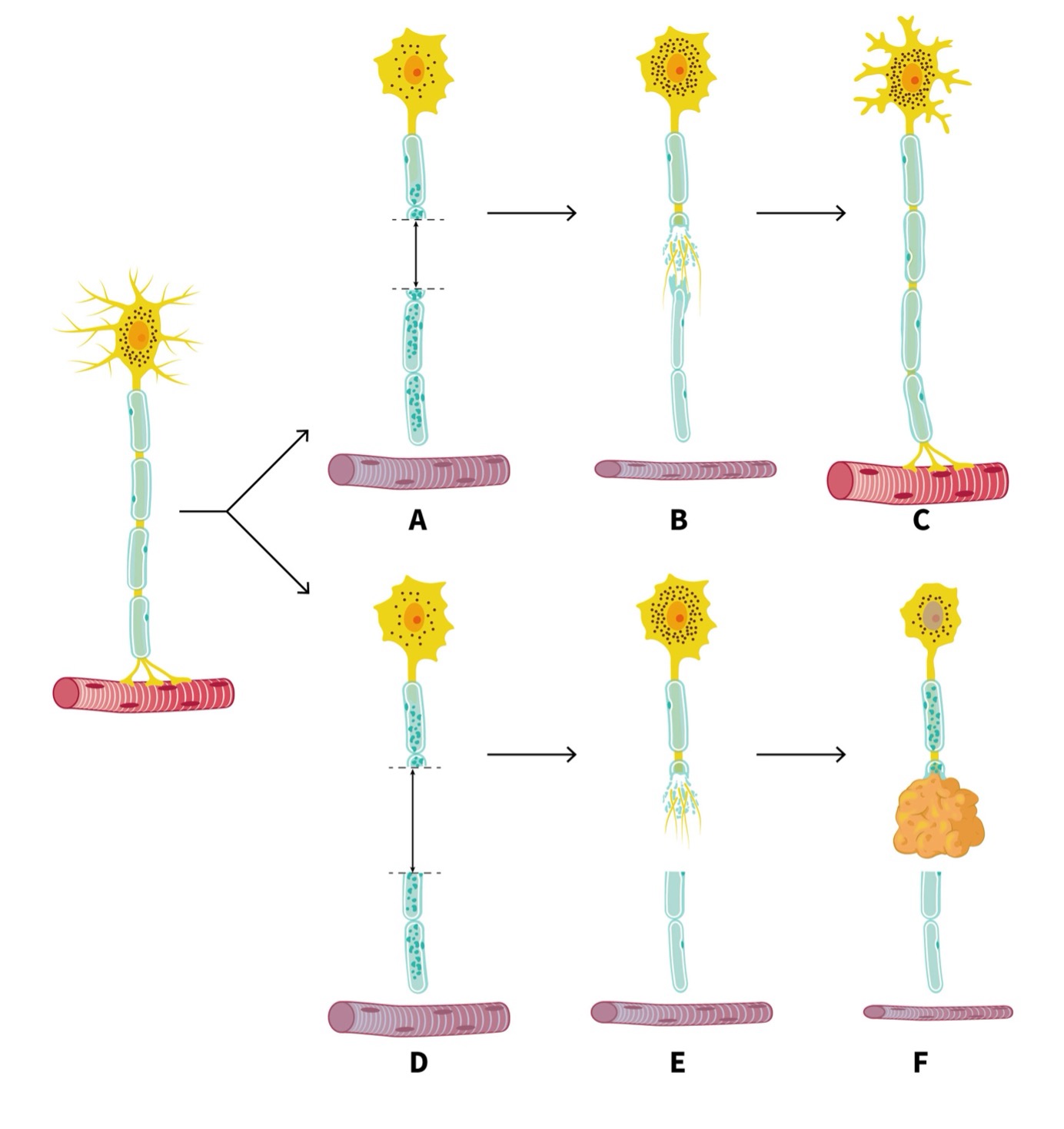
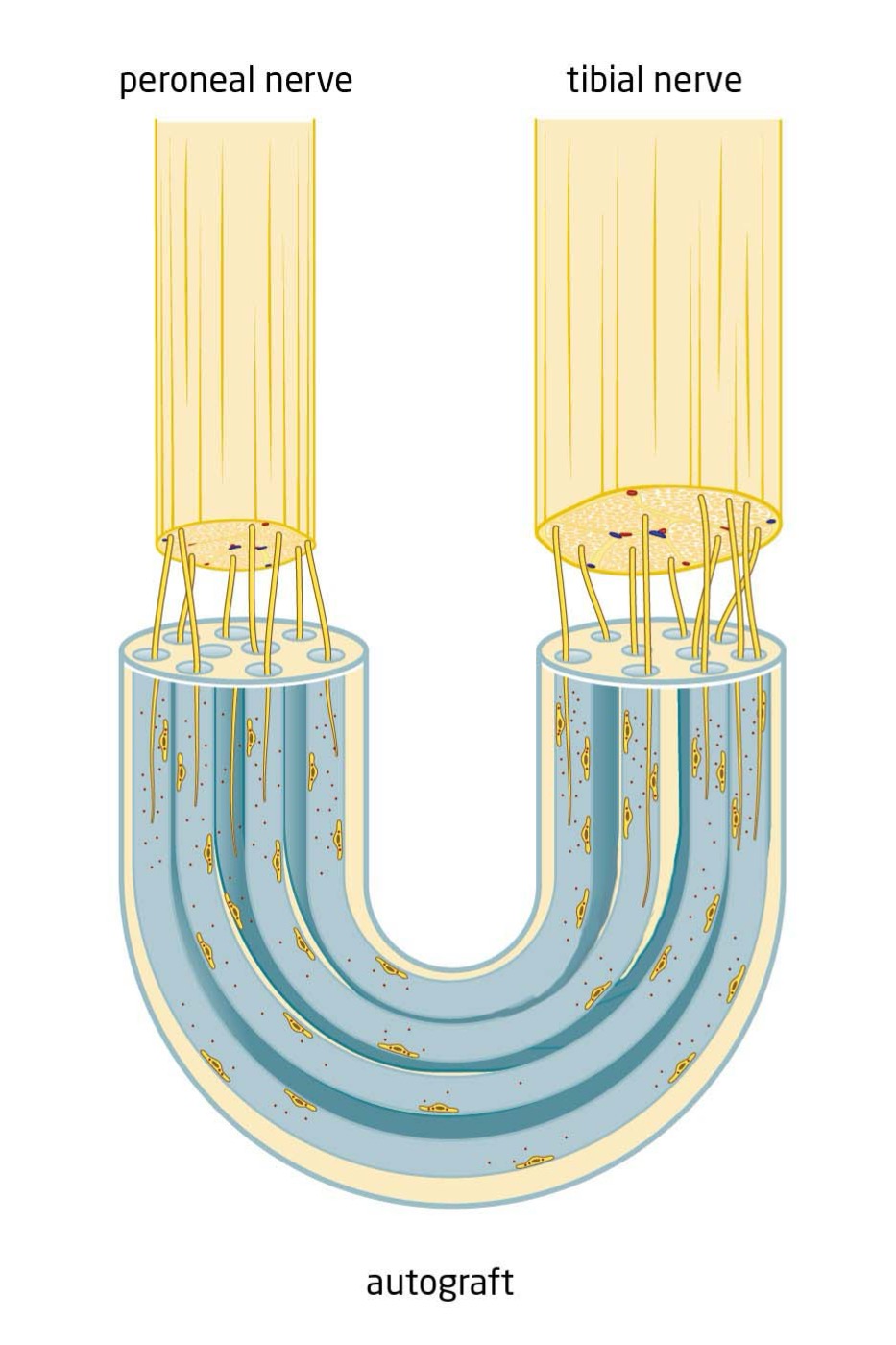
Preventing and treating painful neuromas
Our mission at Atraxon Biotech is to offer a surgical solution for the treatment and prevention of painful neuromas. Neuromas represent one of the most painful neurological conditions worldwide.
Patients develop neuromas after nerve injury or amputation, which can have a big impact on their quality of life. It leads to overuse of pain medication, disrupted rehabilitation, loss of productive years, and high healthcare consumption with high costs involved.